Table of Contents
Does United Healthcare cover wegovy for weight loss? Find out if United Healthcare will pay for your Wegovy weight reduction treatment. Find out if you qualify for Wegovy, what its benefits are, and how to get started on your quest to a healthier weight.
READ MORE: Deciphering the Health Risks Associated with Sugar and Sedentary Lifestyle to Men
Introduction
People frequently investigate a wide range of possibilities, including the use of prescription drugs, in the hope of locating weight loss remedies that are both safe and successful. Wegovy is one of these medications that is garnering a lot of attention.
However, does United Healthcare cover weight reduction treatment with Wegovy? This detailed guide’s goal is to give you with a solution to this issue and insights on Wegovy’s coverage, eligibility requirements, and the role it plays in your path to lose weight.
A Breakthrough Medication for Weight Loss Called Wegovy
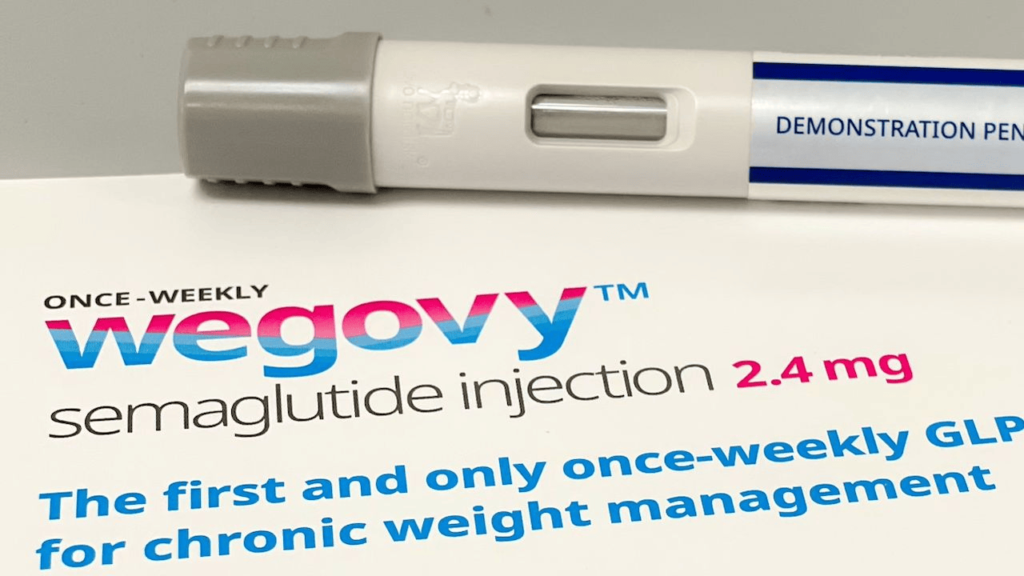
Wegovy, also known by its scientific name semaglutide 2.4 mg, is a weight loss drug that has shown to be a revolutionary breakthrough in recent years. It does this by imitating the activity of a hormone found naturally in the body called GLP-1, which is responsible for helping to manage one’s appetite and the amount of food that they consume.
The Efficiency of the WeGov Platform
In clinical tests, Wegovy demonstrated an impressively high level of effectiveness. individuals who utilized it as part of their program to lose weight saw considerable reductions in their body weight; hence, it is a promising alternative for individuals who are battling with obesity.
Provision of Coverage by United Healthcare
The most pressing issue at hand is whether or not United Healthcare provides coverage for Wegovy for weight loss. The good news is that United Healthcare, along with a large number of other insurance companies, acknowledges the possible advantages of Wegovy and may cover it under specific conditions.
The Criteria for Eligibility
Before you make any hasty plans to obtain a prescription, it is crucial that you have a thorough understanding of the qualifying criteria that United Healthcare has established for Wegovy coverage.
Requirements for One’s Body Mass Index (BMI)
People with a body mass index of 30 or more are normally eligible for coverage under United Healthcare’s Wegovy program. However, if you have other health concerns that are associated with obesity, such as type 2 diabetes, they may consider providing coverage with a lower BMI.
Authorization Ahead of Time
In the majority of instances, in order to prescribe Wegovy, your healthcare provider will be required to seek prior authorization from United Healthcare. This verifies that the drug is required for your condition from a medical standpoint and that it was the right choice.
READ MORE: How Might Food Consumption of Carbs and Fats Affect Men’s vs. Women’s Longevity? (R100)
How to Make Your Way Through the Wegovy Coverage Process
The first thing you need to do is make sure you understand whether or not your insurance policy covers Wegovy. The following is a guide that will assist you in properly navigating the process:
Discussion with Your Preferred Healthcare Professional
To get started, you should make an appointment to see your primary care physician. They will determine whether or not you are eligible for Wegovy and talk to you about the possible benefits and hazards.
Authorization Ahead of Time
Should it be determined that you satisfy the prerequisites for participation, your healthcare provider will start the prior authorization process with United Healthcare on your behalf. Be ready to give any relevant medical data to support your case, and do so as soon as possible.
Taking Expenses Into Account
Although United Healthcare might cover Wegovy, you need to be aware of any out-of-pocket costs, such as copayments or deductibles, that you would be responsible for paying. It is absolutely necessary to have this conversation with both your insurance provider and your healthcare staff.
READ MORE: BREAST ENHANCEMENT – HOW I SAVED TONS OF MONEY WITH BREAST ACTIVES – 40% OFF
(FAQs Of Does United Healthcare Cover Wegovy for Weight Loss?)
Is There a Prescription Available for Wegovy to Help with Cosmetic Weight Loss?
No, Wegovy is not normally recommended for those who do not have obesity or any of the health issues that are associated to obesity. It is not designed to be used for the goal of losing weight for cosmetic reasons.
Are There Any Potential Risks Associated with Taking Wegovy?
Wegovy, like any other medicine, could potentially have adverse effects. Nausea, diarrhea, and constipation are typical adverse reactions that can occur. On the other hand, it’s common for these negative effects to fade away as your body gets used to the medicine.
Is Wegovy a Substitute for a Healthy Diet and Regular Exercise?
Wegovy works best when it is incorporated into a comprehensive plan for weight loss. This approach should also involve maintaining a healthy diet and engaging in regular physical activity. It is not a solution that can stand on its own.
If United Healthcare rejects my request for coverage, do I have the option to appeal?
You do have the opportunity to file an appeal against the decision if you are not granted coverage. To successfully manage the appeals process, it is important to maintain in communication with both your healthcare practitioner and insurance company.
How Much Time Does It Take to Start Seeing Results from Using Wegovy?
Although everyone’s results are different, most people start to notice a considerable reduction in their body weight within the first few months of using Wegovy.
When taking Wegovy, are there any dietary restrictions that need to be followed?
It is imperative that you adhere to the dietary instructions provided by your healthcare professional while you are taking Wegovy. They can recommend some special dietary suggestions to follow in order to get the most out of the drug.
The final word
In conclusion, if you satisfy United Healthcare’s eligibility criteria and obtain prior authorization for Wegovy for weight loss, the insurance provider may pay for your treatment. The use of this drug has showed a great deal of promise in assisting people in accomplishing their weight loss objectives.
To successfully manage the process, however, it is absolutely necessary to maintain close communication with both your healthcare practitioner and insurance company.
It is important to keep in mind that Wegovy is not a stand-alone solution but rather a helpful tool that may be utilized in conjunction with a healthy way of life. If you think that Wegovy could be beneficial to you, talk to your healthcare physician about how to get started on your path to lose weight.




















Leave a Reply